Healthcare Financing and Sustainability
When looking at Healthcare Financing and Sustainability – I think about the cost of care and being good stewards of resources. “Rising healthcare costs and their consequences for Medicare and Medicaid constitute the nation’s central fiscal challenge. Without changes to federal law, the government’s spending on those two programs is on a path that cannot be sustained” from the Congressional Budget Office in 2009 (Longest, 2010; Appendix 8 p 313).
It is estimated that nearly $3.6 TRILLION was spent in 2018 in the U.S., significantly more than any other nation. The concern is that healthcare costs have been and continue to be unsustainable. There is the added concern regarding disparities in health. Though the U.S. is spending trillions of dollars, there are still many Americans who are un- or under- insured.
Impacting Health Policy
When looking to change healthcare policy, specifically Medicare, one must stop to consider, where does the money come from?
Financing of Medicare Part B is primarily achieved through the general fund of the U.S. Treasury, which is funded by Social Security Administration, which is funded by tax dollars (1.45% of your earnings) (Longest, 2010; CNN, 2018). There is also a monthly premium paid by enrollees that contributes to the funding.
Thus, to request that Medicare cover prophylactic mastectomies – this added benefit may come as an additional cost in tax dollars or and increase in the premium paid by Medicare beneficiaries.
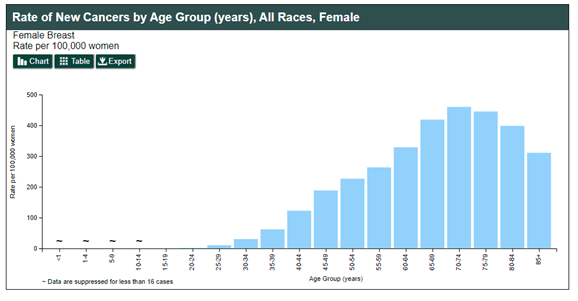
Herein lies the challenge, without a clearly documented benefit of prophylactic mastectomies for Medicare aged women or a defined cost savings for this age group, it is highly unlikely that I will be able to garner enough support from the Health and Human Services committee to move forward with an amendment to Medicare due to the potential increase in spending.
Sustainability
Policy change must be sustainable and cannot only add cost to the current healthcare system, some benefit (decreased cost, improved outcomes) must also be realized. Though I believe that prophylactic mastectomies should be a provided benefit, it will likely come at the cost of the American people.
Perhaps the next best step would be to continue to try to engage with special interest groups, to instill passion and a consensus of the public that breast cancer patients need to have access to prophylactic mastectomies, before attempting to change policy.
References
CNN (2018). Ultimate guide to retirement: Who pays for Medicare? [webpage]. Retrieved from: https://money.cnn.com/retirement/guide/insurance_health.moneymag/index13.htm?iid=EL
Longest, B. B. (2010). Health policymaking in the United States (5th ed.). Chicago, IL: Health administration press.
Sammour, T. (2018, January 25). Healthcare: it is a right or a luxury? A TEDx Adelaide talk . Retrieved from: https://www.youtube.com/watch?v=jCVmY1iOJQs
Schreck, R. (2019, December). Overview of health care financing [webpage]. Retrieved from: https://www.merckmanuals.com/professional/special-subjects/health-care-financing/overview-of-health-care-financing