Ethics and Politics
Ethics – good, just, moral, fair.
Politics – crooked, dirty, dubious, divided.
Ethics and politics are often described at opposite ends of the spectrum, but is there common ground where ethically and politically the goals align? In making decisions and formulating the laws that affect access to medical care I hope that ethics and policy go hand in hand, focusing on beneficence and justice. Quick decisions can be made in policy as described by Kingdon (2003) when Medicare coverage for dialysis and kidney transplant were approved in part due to media coverage of the ethical dilemma of patients not having access to these novel and life saving therapies. However, little thought was given to the significant cost of these treatments. The ethical principle of beneficence should also encompass financial harm. Is the treatment, procedure, or policy cost-effective? As health care providers we must be aware of potential physical, psychological, spiritual, and financial harm. How should ethics influence policy? Universal access, equitable access, affordable access, quality, and choice are the key ethical principles proposed by Gostin (2017) to guide health policy.
So, what about prophylactic mastectomies for women, is there an ethical or political barrier? Yes! Some women choose to have a prophylactic mastectomy if they are at high risk for developing breast cancer (due to genetic mutation). However, more women with breast cancer choose to have a double mastectomy to decrease risk of breast cancer or for other reasons: to avoid radiation, to not have surveillance testing (mammograms, MRI, ultrasounds), or for the peace of knowing that the breast (risk) is removed. I have met women who have had mastectomies to decrease risk, to not have to undergo follow up testing, or for personal reasons. Breast cancer affects women across multiple ages from 40 to 80 as depicted below.
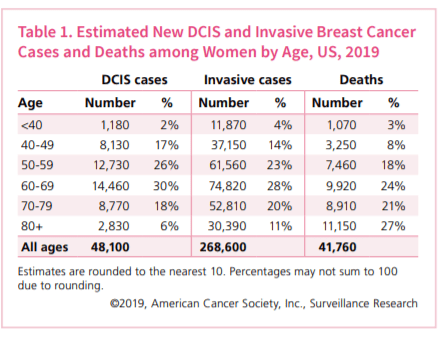
American Cancer Society (2019)
These women will only have the option of a double or prophylactic mastectomy dependent upon their insurance coverage, for those who are 65 with Medicare a prophylactic mastectomy is not an option that is covered. I find it unethical to base treatment options first by what the insurance will cover and second by the goals of the patient. Bound by my nursing ethical principals I believe that these women should have the right to choose the treatment option that best aligns with their goals. Policy for Medicare should be reformed to allow for justice, quality, and the choice for these women in the treatment or prevention of breast cancer.
References
American Cancer Society (2019). Breast cancer facts & figures 2019-2020. Atlanta: American Cancer Society, Inc. Retrieved from https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf
Caruso, C. (2017). Why a growing number of women with breast cancer are choosing double mastectomy. STAT+. Retrieved from https://www.statnews.com/2017/08/29/double-mastectomy-breast-cancer/
Gostin, L. (2017). Five ethical values to guide health system reform. JAMA, 318(22), 2171-2172.
Kingdon, J. W. (2003). The policy primeval soup, In Agendas, alternatives, and public policies. New York, NY:Addison-Wesley educational publishers inc.
Hello Amanda,
I enjoyed reading your informative blog!
I was particularly interested in what the patients’ views or reasons were for having a prophylactic bilateral or even unilateral mastectomy. You mentioned some fundamental rights. Han et al. (2011) add that women can also get anxiety from any future MRI, ultrasound, or mammogram. These women want their reconstructions to match, surgical reconstruction improvements have advanced and improved a lot in the past few years, and some women even have prophylactic mastectomies because they are encouraged by their family or healthcare provider.
I was trying to find the difference in survival rates between women who have prophylactic mastectomies versus those who do not, and it is just so dependent on the type of cancer, family history, age, etc. For example, there is conflicting evidence regarding current mastectomy procedures and outcomes for young women diagnosed with breast cancer, depending on the tumor biology and the diagnostic and treatment environment (Donovan et al., 2017).
I keep thinking that the removal of both breasts is such a significant procedure. However, in many circumstances, as the majority of the literature suggests, having a mastectomy is a good option for women desiring to reduce reoccurrence, even if the reoccurrence rate is only lowered a few percentage points (Han et al., 2011).
Therefore, after careful examination and consideration of the patient by qualified medical professionals has been done, if the patient would likely benefit from an elective mastectomy procedure, meaning it would decrease their likelihood of getting breast cancer or having it return, then it seems insurance should be covering such preventative acts.
Do any insurances currently cover any portion of prophylactic mastectomies? What about the reconstruction that many women choose to do after breast removal?
References
Donovan, C., Bao, J., Gangi, A., Amersi, F., Zhang, X., Giuliano, A., & Chung, A. (2017). Bilateral mastectomy as overtreatment for breast cancer in women age forty years and younger with unilateral operable invasive breast cancer. Annals of Surgical Oncology, 24(8), 2168-2173.
Han, E., Johnson, N., Glissmeyer, M., Wagie, T., Carey, B., Delamelena, T., & Nelson, J. (2011). Increasing incidence of bilateral mastectomies: The patient perspective. The American Journal of Surgery, 201(5), 611-614.
LikeLike
Dear Amanda,
What a compelling read thus far! It is amazing to know that Medicare does cover dialysis and kidney transplant costs. The Centers for Medicare and Medicaid Services (CMS) (1997) cover inpatient and outpatient dialysis needs. Medicare Part B helps pay for cost of equipment, supplies, specific lab tests, and other diagnostics related to the patient treatment (United States, (1997). The treatment composition rates are set in advance upon partnership between CMS and the medical providers/facilities. Medicare is responsible for 80% of the payment. Then, the patient or supplemental insurer is responsible for the other 20%. If the patient requires inpatient dialysis for acute care and not necessarily for maintenance dialysis, Medicare Part A covers the hospital visit.
Those who live with end stage renal disease (ESRD) are 1% of the Medicare population but account for 7% of the Medicare budget (University of California San Francisco, 2020). One year of hemodialysis can cost up to $90,000 and peritoneal dialysis costs about $53,000. The Medicare system is spending about $28 million annually for hemodialysis cost for almost 750,000 people in the United States (University of California San Francisco, 2020). The Kidney project is offering bioartificial kidneys to patients who are on dialysis and not a transplant candidate. This program is projected to save about $15 billion annually. The ESRD incidence rate is projected to rise between 11% and 18%. The number of prevalent patients is projected to be between 690,000 and 1,259,000 (University of California San Francisco, 2020).
Breast cancer statistics show that 1 in 8 women will develop breast cancer. Prophylactic mastectomy cost about $1,292 to $1,993 for contralateral removal, and $15,668 to $21, 342 for bilateral removal (Mattos et al., 2015). By 2020, an estimate of 325,010 invasive and non-invasive new cancers will be diagnosed (BreastCancer.org, 2020). For patients who opt in for prophylactic mastectomy have a 90% survival rate. Unfortunately, this is not covered by Medicare. The cost for breast cancer treatment can cost up to $20.5 million varying on the stage of malignancy and treatment option selected (BreastCancer.org, 2020).
In your post, you discuss that the ethical principle of beneficence should encompass financial harm. At what value point do we consider it financial harm? For example, a patient diagnosed with ESRD their treatment options are dialysis, transplant, or hospice care. For a patient diagnosed with breast cancer their treatment options are surgery, radiation, hormone therapy, chemotherapy, and targeted therapies. As future providers, we present all the information in order to allow a patient to make a sound and fitting decision. Then, we shock them with facts; Medicare will not cover prophylactic mastectomy. The healthcare system has faults and it is not perfect. Ethically, an individual’s life is irreplaceable and money should never be a barrier to medical care. Politically, tax payer dollars are funding Medicare and Medicaid.
It would be ideal that patients can choose treatments options that best align with their goals and not have to worry about the cost. However, where does the funding come from? More tax payer dollars? Appropriation of funding must be intricate, involved, and daunting. The goal is to achieve the greatest good for the greatest number, while creating the least amount of harm or preventing suffering, but where do we set the boundaries?
References
BreastCancer.org. (2020). U.S. Breast Cancer Statistics. Retrieved from https://www.breastcancer.org/symptoms/understand_bc/statistics
Mattos, D. G., Gfrerer, L. S., Reish, R. M., Hughes, K. J., Cetrulo, C. C., Colwell, A., & Liao, E. (2015). Lifetime Costs of Prophylactic Mastectomies and Reconstruction versus Surveillance. Plastic and Reconstructive Surgery, 136(6), 730e-740e. Doi:10.1097/PRS0000000000001763
United States. (1997). Medicare coverage of kidney dialysis and kidney transplant services: A supplement to your Medicare handbook. U.S. Dept. of Health and Human Services, Health Care Financing Administration.
University of California San Francisco. (2020). The Kidney Project. Retrieved form https://pharm.ucsf.edu/kidney/need/statistics
LikeLike
Thank you Mae for your interesting reply,
As you mention, the cost of breast cancer treatment can be very expensive! I am not trying to condone or state that prophylactic mastectomy should be considered for the potential cost saving benefit, but you asked a great question about funding. NCCN guidelines (2020) state that women should be followed with mammograms yearly after treatment for breast cancer, but breastcancer.org (2010) suggests that women should have mammograms twice per year after breast conserving treatment. An additional consideration is the number of women who will also require ultrasound or breast MRI due to history or anatomy to provide sufficient testing. In my experience women are followed with a mammogram to the affected breast twice per year for the first 2 years (often requiring ultrasound or MRI) and annual mammogram to the unaffected breast. Then will complete annual mammograms. The article you mentioned by Mattos and colleagues (2015) found that the lifetime costs of prophylactic mastectomy with reconstruction was less than recommended surveillance costs. The study by Mattos and colleagues (2015) was looking at 45 year old women, so certainly this amount of cost saving may not be realized in older women. On the whole, I do not believe that prophylactic mastectomy would create a significant cost burden but I need to conduct a more thorough review.
Overall, I agree as a nation we spend nearly 50% more on healthcare costs per person compared to similar nations (Sawyer & Cox, 2018). Health care spending concerns are in the news, in political debates, and mentioned in national goals. We have all heard about the Triple Aim (Institute for Healthcare Improvement, 2020). So how do we provide ethical, cost effective care? I think that this will continue to be a moving target as technology advances, costs increase and decrease, and population needs change. As for prophylactic mastectomy, perhaps an additional study to examine costs in medicare aged patients would be a good start.
References
Breastcancer.org (2010). Two mammograms per year better than one after lumpectomy. [webpage]. Retrieved from:https://www.breastcancer.org/research-news/20100513
Institute for Healthcare Improvement (2020). The IHI Triple Aim. [webpage]. Retrieved from: http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx
Mattos, D. G., Gfrerer, L. S., Reish, R. M., Hughes, K. J., Cetrulo, C. C., Colwell, A., & Liao, E. (2015). Lifetime Costs of Prophylactic Mastectomies and Reconstruction versus Surveillance. Plastic and Reconstructive Surgery, 136(6), 730e-740e. Doi:10.1097/PRS0000000000001763
National Comprehensive Cancer Network (2020). NCCN clinical guidelines in oncology: Breast cancer [webpage]. Retrieved from https://www.nccn.org/professionals/physician_gls/default.aspx#breast
Sawyer, B., & Cox, C. (2018). How does health spending in the U.S. compare to other countries? [webpage]. Retrieved from: https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries/#item-start
LikeLike
Hi Michelle,
Yes, there are many things to consider when looking at a prophylactic mastectomy. In reviewing NCCN guidelines (2020)prophylactic mastectomy was not recommended for patients who underwent breast conserving therapy (lumpectomy) for their breast cancer treatment. I can tell you that I just met a women this week who requires 5 months of chemotherapy prior to mastectomy for the affected breast, and expressed that she wants to have a prophylactic mastectomy to reduce her risk of recurrence and because she does not want to undergo chemotherapy again. There are many factors to consider when discussing the risk/benefit of a prophylactic mastectomy and unfortunately, one of those factors is whether or not it would be covered by insurance.
To answer your question to my knowledge most insurance covers mastectomy for the affected breast, as does medicare if medically necessary, and many private insurances cover prophylactic mastectomy. As for reconstruction, there is a federal law Women’s Health and Cancer Rights Act passed in 1998 that requires insurance coverage of reconstruction of the breast removed by a mastectomy and reconstruction of the other breast to restore symmetry (American Cancer Society, 2019). The law does not apply to Medicare and Medicaid, but medicare does cover reconstruction of breast removed by mastectomy for breast cancer (American Cancer Society, 2019).
References
National Comprehensive Cancer Network (2020).NCCN clinical guidelines in oncology: Breast cancer [webpage]. Retrieved from https://www.nccn.org/professionals/physician_gls/default.aspx#breast
American Cancer Society (2019). Women’s health and cancer rights act [webpage]. Retrieved from: https://www.cancer.org/treatment/finding-and-paying-for-treatment/understanding-health-insurance/health-insurance-laws/womens-health-and-cancer-rights-act.html
LikeLike
I find this a very interesting. My sister was among the less than 2 % population, she had breast cancer at the age of 35. She did undergo treatment and had a mastectomy. She got the genetic testing done, though that was fine, how will this influence her only daughter. I myself had gotten mammogram the year my sister found out and thus far, have been fine. I often wonder what would I do if I had breast cancer, or do I get the genetic testing? How will those results affect how I live? It brings me back to my community. I have seen fellow classmates die from colorectal cancer, they are far from being the age of 50, when they should begin CRC screening (CRC), as recommended by the CDC. What if we screened sooner, will they mean more health care costs to keep them healthy? A person has a right to choose health care, but healthcare professionals are obligated to act in the best interest of the patient, yet allow for autonomy (Milton, C., 2015). If my community members want to be screened at a younger age, do we allow for this? Do we lower the age to 35, just because in the last year we had at least 4 individuals die from CRC before they reach the age of 50, for screening? Or do continue to abide by recommendations that don’t particularly pertain to our population.
What should I know about screening? https://www.cdc.gov/cancer/colorectal/basic_info/screening/index.htm
Milton, C. (2015). The ethics of human freedom and healthcare policy: A nursing theoretical perspective. Nurse science quarterly, 28 (3), 192-94. doi: 10.1177/0894318415585630
LikeLike