Medicare was first inacted in 1965 to provide health care coverage to American’s aged 65 and older (Longest, 2010). Once a person reaches age 65 they are eligible to enroll in Medicare or choose to defer these benefits if they have health care insurance through their employer (Roberts, 2018). However, social security benefits cannot be utilized if the person is not enrolled in Medicare (Montgomery, 2020).
Why does Medicare coverage matter for breast cancer patients?
Age, is a known risk factor for breast cancer as seen in the graph below. The incidence of breast cancer begins to rise for women in their 40’s with incidence increasing with age. The majority of women diagnosed with breast cancer are age 65-80.
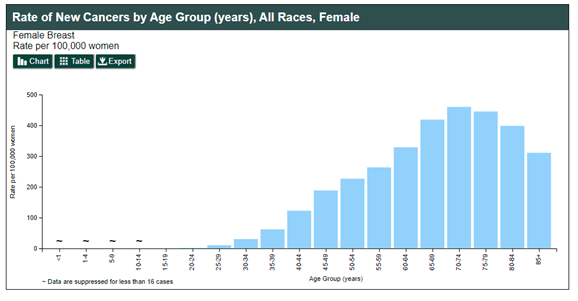
U.S. Cancer Statistics Working Group (2019).
www.cdc.gov/cancer/dataviz
Medicare Part B covers medical services, including outpatient surgery, but for the procedure to be covered it must be either medically necessary or a prescribed preventative benefit (Longest, 2010). A prophylactic mastectomy is defined as a “cosmetic” procedure according to Medicare and not covered.
Financing of Medicare Part B is primarily financed through the general fund of the U.S. Treasury, which is funded by Social Security Administration, which is funded by tax dollars (1.45% of your earnings) (Longest, 2010; CNN, 2018). There is also a monthly premium paid by enrollees that contributes to the funding.
As for spending, Medicare covers cancer treatments including inpatient care, provider visits, chemotherapy, and radiation along with other services. Though patients need to be prepared to pay their 20% deductible.
Inciting change
Medicare is managed at the federal level, thus changes in coverage and policy must occur at the federal level. Questions to be answered would include what is the potential increase in spending? If so, where does the extra money come from? Is there any cost saving benefit? Where is the proof that a prophylactic mastectomy is medically necessary?
I would argue that firstly a prophylactic mastectomy for a breast cancer survivor is not a “cosmetic” procedure. This is a woman who had made the difficult decision to remove a part of her body in the hopes to decrease her cancer risk. Secondly, that prophylactic mastectomy would not cause significant increase in care, as patients with breast cancer require close follow up with mammograms, ultrasounds, and potentially MRIs. One study found that lifetime costs were decreased in women who underwent a prophylactic mastectomy compared to those completing recommended surveillance (Mattos et al., 2015). However, the potential cost savings would need to be further explored with the Medicare aged patients.
There is no black and white answer to is a prophylactic mastectomy medically necessary. There is both support and opposition for this procedure. Like many things in health care, it is a personal, case dependent, decision. However, for a 70-year-old woman on Medicare, this decision is not hers – it was made for her.
And if you think 70 is old or frail.. here are some 70-year old’s – Meryl Streep, Jane Fonda, Tina Turner, Diana Ross, and Cher!
References:
CNN (2018). Ultimate guide to retirement: Who pays for Medicare? [webpage]. Retrieved from: https://money.cnn.com/retirement/guide/insurance_health.moneymag/index13.htm?iid=EL
Longest, B. B. (2010). Health policymaking in the United States (5th ed.). Chicago, IL: Health administration press.
Mattos, D. G., Gfrerer, L. S., Reish, R. M., Hughes, K. J., Cetrulo, C. C., Colwell, A., & Liao, E. (2015). Lifetime Costs of Prophylactic Mastectomies and Reconstruction versus Surveillance. Plastic and Reconstructive Surgery, 136(6), 730e-740e. Doi:10.1097/PRS0000000000001763
Montgomery, K. (2020). Why are you being forced into Medicare at age 65? [webpage]. Retrieved from: https://www.verywellhealth.com/why-am-i-being-forced-into-medicare-at-age-65-1738542
The most stunning women in Hollywood over 70 (2020) [webpage]. Retrieved from: https://www.wonderwall.com/celebrity/photos/most-stunning-women-hollywood-over-70-3011024.gallery
Roberts, D. K. (2018). Is it mandatory to sign up for Medicare at age 65? [webpage]. Retrieved from: https://boomerbenefits.com/is-it-mandatory-to-sign-up-for-medicare-at-age-65/
Roberts, D. K. (2019). How does Medicare cover cancer treatment? [webpage]. Retrieved from: https://boomerbenefits.com/medicares-coverage-for-cancer/
U.S. Cancer Statistics Working Group (2019). U.S. Cancer Statistics Data Visualizations Tool, based on November 2018 submission data (1999-2016): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. Retrieved from www.cdc.gov/cancer/dataviz
Hi Amanda,
I am very interested in your blog topic because my research area tends to be focused on breast cancer survivors, who are the largest, and most homogeneous, group of survivors. I think you bring up a very important point about the long-time classification by Medicare of a prophylactic mastectomy as cosmetic surgery, and the disservice this is to women making such a difficult choice.
There is some very good news that I’d like to pass along to you. In doing assignments for DNP711, I came across a program called the Oncology Care Model, developed within the Medicare (CMS) Innovation Center (CMMIS). OCM is a 5-year feasibility program launched in 2016 to examine the use of payment incentives and best practice care requirements to achieve higher-quality care at lower cost .
As a model, OCM covers payments to providers for care associated with chemotherapy and is triggered once chemotherapy begins. The specifics are that in addition to the usual fee-for-service payments/reimbursements, oncologists and providers who enroll in OCM receive an additional $160/month per survivor if they make the changes required to qualify for OCM. The research intent is two-fold: first, evaluate the feasibility of specific strategies for moving from fee-based services to patient-focused, value-based services; and second, compare quality of care and care costs between the new OCM model and the current Medicare fee-for-service. Comparison data is being gathered from 176 practices in 34 states including about 6,000 oncology providers, who are voluntarily engaged in the OCM feasibility testing, which is about 20% of the fee-for-service population .
The connection between the OCM and prophylactic mastectomy is important because it goes right to the heart of your point about having accurate cost and care information in order to make a good decision.
Because the change-incentive payments start after chemotherapy begins, physicians may be prevented from providing pre-chemotherapy surgery like prophylactic mastectomy. Prophylactic mastectomy in breast cancer is commonly performed, yet Gabrielle Rocque’s team at Genetech suggest that surgery for a mastectomy is associated with higher complication risk and increased spending compared with more conservative surgical approaches .
Meaningful conversations about the risks and benefits of prophylactic mastectomy take time, and time is money in oncology. Survivors would surely benefit by learning more about beneficial, less-aggressive options that could save CMS funds. However, that survivor/physician conversation occurs before chemotherapy, and even today there is no support under OCM to pay for optimal treatment planning at that critical point.
It’s a really complicated issue, and of course every healthcare provider has a different perspective on how to cut costs within their organization. Still, the five years of the study are almost up, and papers with detailed analysis are eagerly anticipated. A lot has been written about OCM and much of it is extensive detail about the calculation of savings and costs, and the validity of the different approaches. It is so detailed that I can’t follow it, but you can get a great overview in the Rocque et al. paper.
Here’s the link: https://ascopubs-org.ezproxy1.lib.asu.edu/doi/10.1200/JOP.2017.024935
1.Kline, R., Adelson, K., Kirshner, J., Strawbridge, L., Devita, M.,Sinanis, N., ….Basch, E. (2017). The Oncology Care Model: Perspectives from the Centers for Medicare & Medicaid Services and participating oncology practices in academia and the community. ASCO (American Society of Clinical Oncology) EDUCATIONAL BOOK, asco.org/edbook.
2.Ibid.
3. Kline, R., Brown, M., Boescher, N., Cox, J., Horenkamp, E., Hoverman, R., ….Strawbridge, L. (2019). The Centers for Medicare & Medicaid Services Oncology Care Model halfway through: Perspectives from diverse participants. Journal of National Cancer Institute (JNCI). 111(8). doi: 10.1093/jnci/djz072.
4. Rocque, G., Williams, C., Kenzik, K., Jackson, B., Halilova, K., Sullivan, M.,….Pisu, M. (2018). Where are the opportunities for reducing health care spending within alternative payment models? Journal of Oncology Practice. 14(6).
LikeLike
Hi Amanda, I didn’t have my name connected to that last post. I’m Nancy Howe, Nancy.Howe@ASU.edu.
LikeLike
Amanda-
That is infuriating. This is yet another example of how women lack bodily autonomy in this society. No women undergo mastectomy for cosmetic reasons. To posit otherwise is ludicrous. These are difficult decisions, made in conjunction with medical professionals. Your point about comparing overall costs between prophylactic mastectomy and required surveillance is telling. Rather than being cost-effective, denying coverage is cost-neutral at best, more expensive at worst. There are also human costs—the increased stress and anxiety that these women experience. Their cancer risk is high, otherwise, they wouldn’t be considering the procedure. Knowing that their lives could be upended at any point has to have a mental health toll on the women and their families.
LikeLike